COBITOLIMOD
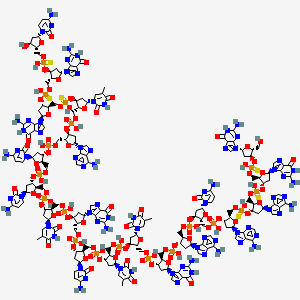
| IUPAC Condensed | dGuo-sP-dGuo-sP-dAdo-sP-dAdo-P-dCyd-P-dAdo-P-dGuo-P-dThd-P-dThd-P-dCyd-P-dGuo-P-dThd-P-dCyd-P-dCyd-P-dAdo-P-dThd-sP-dGuo-sP-dGuo-sP-dCyd |
|---|---|
| Sequence | GGAACAGTTCGTCCATGGC |
| HELM | RNA1{[dR](G).[sp][dR](G).[sp][dR](A).[sp][dR](A).P[dR](C).P[dR](A).P[dR](G).P[dR](T).P[dR](T).P[dR](C).P[dR](G).P[dR](T).P[dR](C).P[dR](C).P[dR](A).P[dR](T).[sp][dR](G).[sp][dR](G).[sp][dR](C)}$$$$ |
| IUPAC | 2′-deoxy-P-thio-guanylyl-(3′->5′)-2′-deoxy-P-thio-guanylyl-(3′->5′)-2′-deoxy-P-thio-adenylyl-(3′->5′)-2′-deoxy-adenylyl-(3′->5′)-2′-deoxy-cytidylyl-(3′->5′)-2′-deoxy-adenylyl-(3′->5′)-2′-deoxy-guanylyl-(3′->5′)-thymidylyl-(3′->5′)-thymidylyl-(3′->5′)-2′-deoxy-cytidylyl-(3′->5′)-2′-deoxy-guanylyl-(3′->5′)-thymidylyl-(3′->5′)-2′-deoxy-cytidylyl-(3′->5′)-2′-deoxy-cytidylyl-(3′->5′)-2′-deoxy-adenylyl-(3′->5′)-P-thio-thymidylyl-(3′->5′)-2′-deoxy-P-thio-guanylyl-(3′->5′)-2′-deoxy-P-thio-guanylyl-(3′->5′)-2′-deoxy-cytidine |
[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-3-[[(2R,3S,5R)-5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[(2R,3S,5R)-5-(2-amino-6-oxo-1H-purin-9-yl)-3-[[(2R,3S,5R)-5-(4-amino-2-oxopyrimidin-1-yl)-3-hydroxyoxolan-2-yl]methoxy-hydroxyphosphinothioyl]oxyoxolan-2-yl]methoxy-hydroxyphosphinothioyl]oxyoxolan-2-yl]methoxy-hydroxyphosphinothioyl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(5-methyl-2,4-dioxopyrimidin-1-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxyoxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(6-aminopurin-9-yl)oxolan-2-yl]methoxy-hydroxyphosphoryl]oxy-5-(4-amino-2-oxopyrimidin-1-yl)oxolan-2-yl]methyl [(2R,3S,5R)-2-[[[(2R,3S,5R)-2-[[[(2R,3S,5R)-5-(2-amino-6-oxo-1H-purin-9-yl)-2-[[[(2R,3S,5R)-5-(2-amino-6-oxo-1H-purin-9-yl)-2-(hydroxymethyl)oxolan-3-yl]oxy-hydroxyphosphinothioyl]oxymethyl]oxolan-3-yl]oxy-hydroxyphosphinothioyl]oxymethyl]-5-(6-aminopurin-9-yl)oxolan-3-yl]oxy-hydroxyphosphinothioyl]oxymethyl]-5-(6-aminopurin-9-yl)oxolan-3-yl] hydrogen phosphate
DNA, d(G-sp-G-sp-A-sp-A-C-A-G-T-T-C-G-T-C-C-A-T-sp-G-sp-G-sp-C)
Molecular Formula, C185-H233-N73-O106-P18-S6
-
Molecular Weight
- 5925.2087
MF C185H233N73O106P18S6
CAS 1226822-98-5
-
WHO 10066,
-
IDX 0150,
-
DIMS 0150,
-
Kappaproct
-
-
-
-
Treatment of Moderate to Severe Ulcerative Colitis
-
DNA based oligonucleotide that activates toll-like receptor 9.
-
UNII: 328101264R
-
DNA, d(g-SP-g-SP-a-SP-a-c-a-g-t-t-c-g-t-c-c-a-t-SP-g-SP-g-SP-C)
Other Names
- DNA d(G-sp-G-sp-A-sp-A-C-A-G-T-T-C-G-T-C-C-A-T-sp-G-sp-G-sp-C)
- 1: PN: WO2007004977 SEQID: 1 claimed DNA
- 1: PN: WO2007050034 PAGE: 29 claimed DNA
- 1: PN: WO2013076262 SEQID: 1 claimed DNA
PATENT
WO/2022/112224COBITOLIMOD DOSAGE FOR SELF-ADMINISTRATION
https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2022112224&_cid=P22-L43JR6-68678-1
Ulcerative colitis (UC) is a disease characterized by chronic inflammation of the rectal and colonic mucosa, affecting the innermost lining in the first stage. The disease is recurrent, with both active and inactive stages that differ in pathology, symptoms and treatment. The underlying cause of UC is not understood, nor is it known what triggers the disease to recur between its inactive and active forms (Irvine, EJ (2008) Inflamm Bowel Dis 14(4): 554-565). Symptoms of active UC include progressive loose stools with blood and increased frequency of bowel movements. Active mucosal inflammation is diagnosed by endoscopy.
The stools contain pus, mucous and blood and are often associated with abdominal cramping with urgency to evacuate (tenesmi). Diarrhoea may have an insidious onset or, more rarely, start quite suddenly. In severe cases the symptoms may include fever and general malaise. In severe stages, deep inflammation of the bowel wall may develop with abdominal tenderness, tachycardia, fever and risk of bowel perforation. Furthermore, patients with UC may suffer extra intestinal manifestations such as arthralgia and arthritis, erythema nodosum, pyoderma gangrenosum and inflammation in the eyes. In the case of remission or inactive UC, patients are usually free of bowel symptoms.
The extent of inflamed and damaged mucosa differs among patients with UC. UC that affects only the rectum is termed ulcerative proctitis. The condition is referred to as distal or left sided colitis when inflammatory changes are present in the left side of the colon up to the splenic flexure. In extensive UC the transverse colon is also affected, and pancolitis designates a disease involving the entire colon.
Active mucosal inflammation is diagnosed by endoscopy and is characterized by a loss of vascular patterning, oedema, petechia, spontaneous bleeding and fibrinous exudates. The endoscopic picture is that of continuous inflammation, starting in the rectum and extending proximally to a variable extent into the colon. Biopsies obtained at endoscopy and subjected to histological examination help to diagnose the condition. Infectious causes, including Clostridium difficile, camphylobacter, Salmonella and Shigella, may mimic UC and can be excluded by stool cultures.
The medical management of UC is divided into treatment of active disease and maintenance of remission.
The treatment of patients with active UC aims to reduce inflammation and promote colon healing and mucosal recovery. In milder cases the disease may be controlled with conventional drugs including sulphasalazine, 5 -aminosalicylic acid (5-ASA) (Sutherland, L., F. Martin, S. Greer, M. Robinson, N. Greenberger, F. Saibil, T Martin, J. Sparr, E. Prokipchuk and L. Borgn (1987) Gastroenterology 92: 1894-1898) and glucocorticosteroids (GCS) (Domenech, E., M. Manosa and E. Cabre (2014). Dig Dis 32( 4): 320-327).
GCS are generally used to treat disease flare-ups and are not recommended for maintenance of remission since there are significant side effects in long-term use, and the possible development of steroid dependent disease. Glucocorticoid drugs act non-selectively, so in the long run they may impair many healthy anabolic processes. As a result, maintenance treatment with systemic GCS is not advised (Prantera, C. and S.
Marconi (2013) Therap Adv Gastroenterol 6(2): 137-156).
For patients who become refractory to GCS and suffer from severe or moderately severe attacks of UC, the addition of immunomodulatory agents such as cyclosporine, 6-mercaptopurine and azathioprine may be used. However, immunomodulators are slow-
acting and the induction of remission in these patients is often temporary (Khan, KJ, MC Dubinsky, AC Ford, TA Ullman, NJ Talley and P. Moayyedi (2011) Am J Gastroenterol 106(4): 630-642).
Further treatment options for UC include biologic agents (Fausel, R. and A. Afzali (2015) Ther Clin Risk Manag 11: 63-73). The three TNF-α inhibitors currently approved for the treatment of moderate to severe UC are infliximab, adalimumab, and golimumab. All three carry potential risks associated with their use, and should be avoided in certain patients, eg those with uncontrolled infections, advanced heart failure, neurologic conditions and in patients with a history of malignancy, due to a potential risk of accelerating the growth of a tumor. Other potential adverse effects of TNF-α inhibitor therapy include neutropenia, hepatotoxicity, serum sickness, leukocytoclastic vasculitis, rash including psoriasiform rash, induction of autoimmunity, and injection or infusion site reactions, including anaphylaxis, convulsions, and hypotension.
All three TNF-α inhibitor agents and their related biosimilar/derivative counterparts may be used to induce and maintain clinical response and remission in patients with UC.
Combination therapy with azathioprine is also used for inducing remission.
However, more than 50% of patients receiving TNF-α inhibitor agents fail to respond to induction dosing, or lose response to the TNF-α inhibitor agents over time (Fausel, R. and A. Afzali (2015) Ther Clin Risk Manag 11 : 63-73).
Vedolizumab, an a4b7 integrin inhibitor, was recently approved for the treatment of UC. In the GEMINI 1 trial, vedolizumab was found to be more effective than placebo for inducing and maintaining clinical response, clinical remission, and mucosal healing (Feagan, BG, P. Rutgeerts, BE Sands, S. Hanauer, JF Colombel, WJ Sandbom, G. Van Assche, J. Axler, HJ Kim, S. Danese, I. Fox, C. Milch, S. Sankoh, T. Wyant, J. Xu, A. Parikh and GS Group (2013) “Vedolizumab as induction and maintenance therapy for ulcerative colitis.” N Engl J Med 369(8): 699-710.).
Ulcerative colitis patients, who are chronically active and refractory to known treatments pose a serious medical challenge and often the only remaining course of action is
colectomy. A total colectomy is a potentially curative option in severe UC, but is a life-changing operation that entails risks as complications, such as pouch failure, pouchitis, pelvic sepsis, infertility in women, and nocturnal faecal soiling, may follow. Therefore, surgery is usually reserved for patients with severe refractory disease, surgical or other emergencies, or patients with colorectal dysplasia or cancer.
An emerging third line treatment for UC is cobitolimod (Kappaproct/DIMS0150), a modified single strand deoxyribonucleic acid (DNA)-based synthetic oligonucleotide of 19 bases in length. Cobitolimod has the sequence 5′- G*G*A*ACAGTTCGTCCAT*G*G*C-3′ (SEQ ID NO:1), wherein the CG dinucleotide is unmethylated.
Cobitolimod functions as an immunomodulatory agent by targeting the Toll-like receptor 9 (TLR9) present in immune cells. These immune cells (ie, B-cells and plasmacytoid dendritic cell (pDCs) reside in high abundance in mucosal surfaces, such as colonic and nasal mucosa. The immune system is the key mediator of the changes of UC. The mucosa of the colon and rectum of patients with UC is chronically inflamed and contains active immune cells. Cobitolimod may be topically administered in the region of inflammation, which places the drug in close contact with a high number of intended target cells, ensuring that the drug will reach an area rich in TLR9 expressing cells.The activation of these cells by cobitolimod induces various cytokines,
The clinical efficacy of cobitolimod has been demonstrated in the “COLLECT” (CSUC-01/10 ) clinical trial, which involved the administration to patients of 30 mg doses of cobitolimod, at 4 week intervals and also in the “CONDUCT” (CSUC- 01/16 ) clinical trial, which involved testing different dosage regimes. The details of the “COLLECT” trial were published in Journal of Crohn’s and Colitis (Atreya et al. J Crohn’s Colitis, 2016 May 20) and are summarized in Reference Example 1. The details of the “CONDUCT” clinical trial were published in The Lancet Gastroenterology and Hepatology (Atreya et al 2020. Lancet Gastroenterol Hepatol. 2020 Dec;5(12): 1063-1075) and are summarized in Reference Example 2. Overall, data on cobitolimod support a positive benefit-risk
assessment for patients with chronic UC which is in an active phase (occasionally referred to herein as “chronic active UC”). Cobitolimod is safe and well tolerated and has been shown to be effective to induce clinical response and remission in patients with chronic UC which is in an active phase, as well as symptomatic and endoscopic remission in patients with treatment refractory, moderate to severe chronic UC which is in an active phase. Despite the clinical trial results obtained this far, there still remains a need for additional effective dosages of cobitolimod which exhibit both good efficacy and safety.
In the COLLECT study, which involved administration of a relatively low (30mg) dose of cobitolimod, topical administration of cobitolimod was performed using a spray catheter device, administered during an endoscopy. This is an invasive medical procedure which is necessarily carried out by a medical professional. Further, before the topical administration of the cobitolimod to the patients, the colon of each patient was cleaned to remove faecal matter. That was done to enable the cobitolimod to reach the intestinal epithelial cells within the colon and to enable the endoscopist to view the colonic mucosa. Thus, it is well known in the art that oligonucleotides such as cobitolimod bind to organic matter such as faeces.
As noted above, patients suffering from chronic ulcerative colitis, who are in an active disease state and refractory to known treatments pose a serious medical challenge and often the only remaining course of action is colectomy. For this reason, patients will tolerate medical intervention which requires both colonic cleaning to remove faecal matter and topical administration via spray catheter, despite the inconvenience and discomfort involved in such invasive procedures. However, it would be therapeutically desirable to provide a topical treatment for ulcerative colitis patients which does not require colonic cleaning to remove faecal matter and which, preferably, can be self-administered by the patient.
PATENTS
-
WO2001074344
-
WO2005080568
-
WO2007004977
-
WO2007004979
-
WO2007050034
-
EP2596806
-
WO2018206722
- WO2018206713
-
WO2018206711
-
WO2020099585
-
WO2021037764
//////////

AS ON DEC2021 3,491,869 VIEWS ON BLOG WORLDREACH AVAILABLEFOR YOUR ADVERTISEMENT

join me on Linkedin
Anthony Melvin Crasto Ph.D – India | LinkedIn
join me on Researchgate
RESEARCHGATE

join me on Facebook
Anthony Melvin Crasto Dr. | Facebook
join me on twitter
Anthony Melvin Crasto Dr. | twitter
+919321316780 call whatsaapp
EMAIL. amcrasto@amcrasto
/////////////////////////////////////////////////////////////////////////////
InDex Pharmaceuticals enters phase III study of the drug candidate cobitolimod
InDex Pharmaceuticals enters agreement with Parexel Biotech for phase III clinical study of cobitolimod for ulcerative colitis
InDex Pharmaceuticals Holding AB (publ) announced that the company has entered an agreement for services with global clinical research organisation (CRO) Parexel Biotech for the phase III study CONCLUDE. The study will evaluate the efficacy and safety of the drug candidate cobitolimod for the treatment of moderate to severe left-sided ulcerative colitis.
“We are excited to advance cobitolimod into phase III, which is the final stage of development before applying for market approval. After the successful collaboration in our recent phase IIb study CONDUCT, we are very pleased to collaborate once again with Parexel Biotech as our clinical development partner”, says Peter Zerhouni, CEO of InDex Pharmaceuticals. “Parexel Biotech is a leading global CRO with considerable experience managing phase III studies in inflammatory bowel disease, which will ensure an efficient execution of the study.”
CONCLUDE is a randomised, double-blind, placebo-controlled, global phase III study to evaluate cobitolimod as a novel treatment for patients with moderate to severe left-sided ulcerative colitis. The induction study will include approximately 400 patients, and the primary endpoint will be clinical remission at week 6. Patients responding to cobitolimod in the induction study will be eligible to continue in a one-year maintenance study, where they will be treated with either cobitolimod or a placebo.
Apart from the dosing 250 mg x 2, which was the highest dose and the one that showed the best efficacy in the phase IIb study CONDUCT, the phase III study will also evaluate a higher dose, 500 mg x 2, in an adaptive study design. This higher dose has the potential to provide even better efficacy than what was observed in the phase IIb study.
“We are pleased to partner with InDex Pharmaceuticals on phase III clinical trial CONCLUDE to evaluate a potential new therapy for patients with moderate to severe ulcerative colitis,” said Jim Anthony, Senior Vice President and Global Head, Parexel Biotech. “Our collaboration with InDex Pharmaceuticals demonstrates our commitment to designing innovative solutions that draw from our global clinical experience and therapeutic expertise to fulfil unmet medical needs on behalf of patients worldwide.”
///////////COBITOLIMOD, WHO 10066, IDX 0150, DIMS 0150, Kappaproct
CC1=CN(C(=O)NC1=O)C2CC(C(O2)COP(=O)(O)OC3CC(OC3COP(=O)(O)OC4CC(OC4COP(=O)(O)OC5CC(OC5COP(=O)(O)OC6CC(OC6COP(=O)(O)OC7CC(OC7COP(=S)(O)OC8CC(OC8COP(=S)(O)OC9CC(OC9COP(=S)(O)OC1CC(OC1CO)N1C=NC2=C1N=C(NC2=O)N)N1C=NC2=C1N=C(NC2=O)N)N1C=NC2=C(N=CN=C21)N)N1C=NC2=C(N=CN=C21)N)N1C=CC(=NC1=O)N)N1C=NC2=C(N=CN=C21)N)N1C=NC2=C1N=C(NC2=O)N)N1C=C(C(=O)NC1=O)C)OP(=O)(O)OCC1C(CC(O1)N1C=CC(=NC1=O)N)OP(=O)(O)OCC1C(CC(O1)N1C=NC2=C1N=C(NC2=O)N)OP(=O)(O)OCC1C(CC(O1)N1C=C(C(=O)NC1=O)C)OP(=O)(O)OCC1C(CC(O1)N1C=CC(=NC1=O)N)OP(=O)(O)OCC1C(CC(O1)N1C=CC(=NC1=O)N)OP(=O)(O)OCC1C(CC(O1)N1C=NC2=C(N=CN=C21)N)OP(=O)(O)OCC1C(CC(O1)N1C=C(C(=O)NC1=O)C)OP(=S)(O)OCC1C(CC(O1)N1C=NC2=C1N=C(NC2=O)N)OP(=S)(O)OCC1C(CC(O1)N1C=NC2=C1N=C(NC2=O)N)OP(=S)(O)OCC1C(CC(O1)N1C=CC(=NC1=O)N)O
Smiles
CC1=CN([C@H]2C[C@H](OP(=O)