The U.S. Food and Drug Administration today granted accelerated approval to benznidazole for use in children ages 2 to 12 years old with Chagas disease. It is the first treatment approved in the United States for the treatment of Chagas disease.
Chagas disease, or American trypanosomiasis, is a parasitic infection caused by Trypanosoma cruzi and can be transmitted through different routes, including contact with the feces of a certain insect, blood transfusions, or from a mother to her child during pregnancy. After years of infection, the disease can cause serious heart illness, and it also can affect swallowing and digestion. While Chagas disease primarily affects people living in rural parts of Latin America, recent estimates are that there may be approximately 300,000 persons in the United States with Chagas disease.
“The FDA is committed to making available safe and effective therapeutic options to treat tropical diseases,” said Edward Cox, M.D., director of the Office of Antimicrobial Products in the FDA’s Center for Drug Evaluation and Research.
The safety and efficacy of benznidazole were established in two placebo-controlled clinical trials in pediatric patients 6 to 12 years old. In the first trial, approximately 60 percent of children treated with benznidazole had an antibody test change from positive to negative compared with approximately 14 percent of children who received a placebo. Results in the second trial were similar: Approximately 55 percent of children treated with benznidazole had an antibody test change from positive to negative compared with 5 percent who received a placebo. An additional study of the safety and pharmacokinetics (how the body absorbs, distributes and clears the drug) of benznidazole in pediatric patients 2 to 12 years of age provided information for dosing recommendations down to 2 years of age.
The most common adverse reactions in patients taking benznidazole were stomach pain, rash, decreased weight, headache, nausea, vomiting, abnormal white blood cell count, urticaria (hives), pruritus (itching) and decreased appetite. Benznidazole is associated with serious risks including serious skin reactions, nervous system effects and bone marrow depression. Based on findings from animal studies, benznidazole could cause fetal harm when administered to a pregnant woman.
Benznidazole was approved using the Accelerated Approval pathway. The Accelerated Approval pathway allows the FDA to approve drugs for serious conditions where there is unmet medical need and adequate and well-controlled trials establish that the drug has an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients. Further study is required to verify and describe the anticipated clinical benefit of benznidazole.
The FDA granted benznidazole priority review and orphan product designation. These designations were granted because Chagas disease is a rare disease, and until now, there were no approved drugs for Chagas disease in the United States.
With this approval, benznidazole’s manufacturer, Chemo Research, S. L., is awarded a Tropical Disease Priority Review Voucher in accordance with a provision included in the Food and Drug Administration Amendments Act of 2007 that aims to encourage development of new drugs and biological products for the prevention and treatment of certain tropical diseases.
 |
|
| Clinical data | |
|---|---|
| Trade names | Rochagan, Radanil[1] |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| Routes of administration |
by mouth |
| ATC code | |
| Pharmacokinetic data | |
| Bioavailability | High |
| Metabolism | Liver |
| Biological half-life | 12 hours |
| Excretion | Kidney and fecal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard | 100.153.448 |
| Chemical and physical data | |
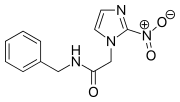
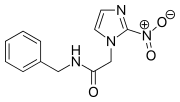
| Formula | C12H12N4O3 |
| Molar mass | 260.249 g/mol |
| 3D model (JSmol) | |
| Melting point | 188.5 to 190 °C (371.3 to 374.0 °F) |
Benznidazole is an antiparasitic medication used in the treatment of Chagas disease.[2] While it is highly effective in early disease this decreases in those who have long term infection.[3] It is the first line treatment given its moderate side effects compared to nifurtimox.[1] It is taken by mouth.[2]
Side effects are fairly common. They include rash, numbness, fever, muscle pain, loss of appetite, and trouble sleeping.[4][5] Rare side effects include bone marrow suppression which can lead to low blood cell levels.[1][5] It is not recommended during pregnancy or in people with severe liver or kidney disease.[4][3]Benznidazole is in the nitroimidazole family of medication and works by the production of free radicals.[5][6]
Benznidazole came into medical use in 1971.[2] It is on the World Health Organization’s List of Essential Medicines, the most effective and safe medicines needed in a health system.[7] It is not commercially available in the United States, but can be obtained from the Centers of Disease Control.[2] As of 2012 Laboratório Farmacêutico do Estado de Pernambuco, a government run pharmaceutical company in Brazil was the only producer.[8]
Medical uses
Benznidazole has a significant activity during the acute phase of Chagas disease, with a therapeutical success rate up to 80%. Its curative capabilities during the chronic phase are, however, limited. Some studies have found parasitologic cure (a complete elimination of T. cruzi from the body) in pediatric and young patients during the early stage of the chronic phase, but overall failure rate in chronically infected individuals is typically above 80%.[6]
However, some studies indicate treatment with benznidazole during the chronic phase, even if incapable of producing parasitologic cure, because it reduces electrocardiographic changes and a delays worsening of the clinical condition of the patient.[6]
Benznidazole has proven to be effective in the treatment of reactivated T. cruzi infections caused by immunosuppression, such as in people with AIDS or in those under immunosuppressive therapy related to organ transplants.[6]
Children
Benznidazole can be used in children and infants, with the same 5–7 mg/kg per day weight-based dosing regimen that is used to treat adult infections.[9] Children are found to be at a lower risk of adverse events compared to adults, possibly due to increased hepatic clearance of the drug. The most prevalent adverse effects in children were found to be gastrointestinal, dermatologic, and neurologic in nature. However, the incidence of severe dermatologic and neurologic adverse events is lower in the pediatric population compared to adults.[10]
Pregnant women
Studies in animals have shown that benznidazole can cross the placenta.[11] Due to its potential for teratogenicity, use of benznidazole in pregnancy is not recommended.[9]
Side effects
Side effects tend to be common and occur more frequently with increased age.[12] The most common adverse reactions associated with benznidazole are allergic dermatitis and peripheral neuropathy.[1] It is reported that up to 30% of people will experience dermatitis when starting treatment.[11][13] Benznidazole may cause photosensitization of the skin, resulting in rashes.[1] Rashes usually appear within the first 2 weeks of treatment and resolve over time.[13] In rare instances, skin hypersensitivity can result in exfoliative skin eruptions, edema, and fever.[13] Peripheral neuropathy may occur later on in the treatment course and is dose dependent.[1] It is not permanent, but takes time to resolve.[13]
Other adverse reactions include anorexia, weight loss, nausea, vomiting, insomnia, and dysguesia, and bone marrow suppression.[1] Gastrointestinal symptoms usually occur during the initial stages of treatment and resolves over time.[13] Bone marrow suppression has been linked to the cumulative dose exposure.[13]
Contraindications
Benznidazole should not be used in people with severe liver and/or kidney disease.[12] Pregnant women should not use benznidazole because it can cross the placenta and cause teratogenicity.[11]
Pharmacology
Mechanism of action
Benznidazole is a nitroimidazole antiparasitic with good activity against acute infection with Trypanosoma cruzi, commonly referred to as Chagas disease.[11] Like other nitroimidazoles, benznidazole’s main mechanism of action is to generate radical species which can damage the parasite’s DNA or cellular machinery.[14] The mechanism by which nitroimidazoles do this seems to depend on whether or not oxygen is present.[15] This is particularly relevant in the case of Trypanosoma species, which are considered facultative anaerobes.[16]
Under anaerobic conditions, the nitro group of nitroimidazoles is believed to be reduced by the pyruvate:ferredoxin oxidoreductase complex to create a reactive nitro radical species.[14] The nitro radical can then either engage in other redox reactions directly or spontaneously give rise to a nitrite ion and imidazole radical instead.[15] The initial reduction takes place because nitroimidazoles are better electron acceptors for ferredoxin than the natural substrates.[14] In mammals, the principal mediators of electron transport are NAD+/NADH and NADP+/NADPH, which have a more positive reduction potential and so will not reduce nitroimidazoles to the radical form.[14] This limits the spectrum of activity of nitroimidazoles so that host cells and DNA are not also damaged. This mechanism has been well-established for 5-nitroimidazoles such as metronidazole, but it is unclear if the same mechanism can be expanded to 2-nitroimidazoles (including benznidazole).[15]
In the presence of oxygen, by contrast, any radical nitro compounds produced will be rapidly oxidized by molecular oxygen, yielding the original nitroimidazole compound and a superoxide anion in a process known as “futile cycling“.[14] In these cases, the generation of superoxide is believed to give rise to other reactive oxygen species.[15] The degree of toxicity or mutagenicity produced by these oxygen radicals depends on cells’ ability to detoxify superoxide radicals and other reactive oxygen species.[15] In mammals, these radicals can be converted safely to hydrogen peroxide, meaning benznidazole has very limited direct toxicity to human cells.[15] In Trypanosoma species, however, there is a reduced capacity to detoxify these radicals, which results in damage to the parasite’s cellular machinery.[15]
Pharmacokinetics
Oral benznidazole has a bioavailability of 92%, with a peak concentration time of 3–4 hours after administration.[17] 5% of the parent drug is excreted unchanged in the urine, which implies that clearance of benznidazole is mainly through metabolism by the liver.[18] Its elimination half-life is 10.5-13.6 hours.[17]
Interactions
Benznidazole and other nitroimidazoles have been shown to decrease the rate of clearance of 5-fluorouracil (including 5-fluorouracil produced from its prodrugs capecitabine, doxifluridine, and tegafur).[19]While co-administration of any of these drugs with benznidazole is not contraindicated, monitoring for 5-fluorouracil toxicity is recommended in the event they are used together.[20]
The GLP-1 receptor agonist lixisenatide may slow down the absorption and activity of benznidazole, presumably due to delayed gastric emptying.[21]
Because nitroimidazoles can kill Vibrio cholerae cells, use is not recommended within 14 days of receiving a live cholera vaccine.[22]
Alcohol consumption can cause a disulfiram like reaction with benznidazole.[1]
References
- ^ Jump up to:a b c d e f g h Bern, Caryn; Montgomery, Susan P.; Herwaldt, Barbara L.; Rassi, Anis; Marin-Neto, Jose Antonio; Dantas, Roberto O.; Maguire, James H.; Acquatella, Harry; Morillo, Carlos (2007-11-14). “Evaluation and Treatment of Chagas Disease in the United States: A Systematic Review”. JAMA. 298 (18): 2171–81. ISSN 0098-7484. PMID 18000201. doi:10.1001/jama.298.18.2171.
- ^ Jump up to:a b c d “Our Formulary | Infectious Diseases Laboratories | CDC”. www.cdc.gov. 22 September 2016. Retrieved 7 December2016.
- ^ Jump up to:a b “Chagas disease”. World Health Organization. March 2016. Retrieved 7 December 2016.
- ^ Jump up to:a b Prevention, CDC – Centers for Disease Control and. “CDC – Chagas Disease – Resources for Health Professionals – Antiparasitic Treatment”. www.cdc.gov. Retrieved 2016-11-05.
- ^ Jump up to:a b c Castro, José A.; de Mecca, Maria Montalto; Bartel, Laura C. (2006-08-01). “Toxic side effects of drugs used to treat Chagas’ disease (American trypanosomiasis)”. Human & Experimental Toxicology. 25 (8): 471–479. ISSN 0960-3271. PMID 16937919. doi:10.1191/0960327106het653oa.
- ^ Jump up to:a b c d Urbina, Julio A. “Nuevas drogas para el tratamiento etiológico de la Enfermedad de Chagas” (in Spanish). Retrieved March 24, 2012.
- Jump up^ “WHO Model List of Essential Medicines (19th List)” (PDF). World Health Organization. April 2015. Retrieved 8 December 2016.
- Jump up^ “Treatment for Chagas: Enter Supplier Number Two | End the Neglect”. endtheneglect.org. 21 March 2012. Retrieved 7 December 2016.
- ^ Jump up to:a b Carlier, Yves; Torrico, Faustino; Sosa-Estani, Sergio; Russomando, Graciela; Luquetti, Alejandro; Freilij, Hector; Vinas, Pedro Albajar (2011-10-25). “Congenital Chagas Disease: Recommendations for Diagnosis, Treatment and Control of Newborns, Siblings and Pregnant Women”. PLOS Negl Trop Dis. 5 (10): e1250. ISSN 1935-2735. PMC 3201907
 . PMID 22039554. doi:10.1371/journal.pntd.0001250.
. PMID 22039554. doi:10.1371/journal.pntd.0001250. - Jump up^ Altcheh, Jaime; Moscatelli, Guillermo; Moroni, Samanta; Garcia-Bournissen, Facundo; Freilij, Hector (2011-01-01). “Adverse Events After the Use of Benznidazole in Infants and Children With Chagas Disease”. Pediatrics. 127 (1): e212–e218. ISSN 0031-4005. PMID 21173000. doi:10.1542/peds.2010-1172.
- ^ Jump up to:a b c d Pérez-Molina, José A.; Pérez-Ayala, Ana; Moreno, Santiago; Fernández-González, M. Carmen; Zamora, Javier; López-Velez, Rogelio (2009-12-01). “Use of benznidazole to treat chronic Chagas’ disease: a systematic review with a meta-analysis”. Journal of Antimicrobial Chemotherapy. 64 (6): 1139–1147. ISSN 0305-7453. PMID 19819909. doi:10.1093/jac/dkp357.
- ^ Jump up to:a b Prevention, CDC – Centers for Disease Control and. “CDC – Chagas Disease – Resources for Health Professionals – Antiparasitic Treatment”. www.cdc.gov. Retrieved 2016-11-07.
- ^ Jump up to:a b c d e f Grayson, M. Lindsay; Crowe, Suzanne M.; McCarthy, James S.; Mills, John; Mouton, Johan W.; Norrby, S. Ragnar; Paterson, David L.; Pfaller, Michael A. (2010-10-29). Kucers’ The Use of Antibiotics Sixth Edition: A Clinical Review of Antibacterial, Antifungal and Antiviral Drugs. CRC Press. ISBN 9781444147520.
- ^ Jump up to:a b c d e Edwards, David I (1993). “Nitroimidazole drugs – action and resistance mechanisms. I. Mechanism of action”. Journal of Antimicrobial Chemotherapy. 31: 9–20. doi:10.1093/jac/31.1.9.
- ^ Jump up to:a b c d e f g Eller, Gernot. “Synthetic Nitroimidazoles: Biological Activities and Mutagenicity Relationships”. Scientia Pharmaceutica. 77: 497–520. doi:10.3797/scipharm.0907-14.
- Jump up^ Cheng, Thomas C. (1986). General Parasitology. Orlando, Florida: Academic Press. p. 140. ISBN 0-12-170755-5.
- ^ Jump up to:a b Raaflaub, J; Ziegler, WH (1979). “Single-dose pharmacokinetics of the trypanosomicide benznidazole in man”. Arzneimittelforschung. 29 (10): 1611–1614.
- Jump up^ Workman, P.; White, R. A.; Walton, M. I.; Owen, L. N.; Twentyman, P. R. (1984-09-01). “Preclinical pharmacokinetics of benznidazole.”. British Journal of Cancer. 50 (3): 291–303. ISSN 0007-0920. PMC 1976805
 . PMID 6466543. doi:10.1038/bjc.1984.176.
. PMID 6466543. doi:10.1038/bjc.1984.176. - Jump up^ Product Information: Teysuno oral capsules, tegafur gimeracil oteracil oral capsules. Nordic Group BV (per EMA), Hoofddorp, The Netherlands, 2012.
- Jump up^ Product Information: TINDAMAX(R) oral tablets, tinidazole oral tablets. Mission Pharmacal Company, San Antonio, TX, 2007.
- Jump up^ Product Information: ADLYXIN(TM) subcutaneous injection, lixisenatide subcutaneous injection. sanofi-aventis US LLC (per manufacturer), Bridgewater, NJ, 2016.
- Jump up^ Product Information: VAXCHORA(TM) oral suspension, cholera vaccine live oral suspension. PaxVax Inc (per manufacturer), Redwood City, CA, 2016.
External links
- “Rochagan [Patient Information]” (PDF) (in Portuguese). Hoffmann-La Roche. Retrieved 2006-11-27.
////////////benznidazole, Chemo Research, Tropical Disease Priority Review Voucher, Chagas disease, rare disease, FDA 2017














